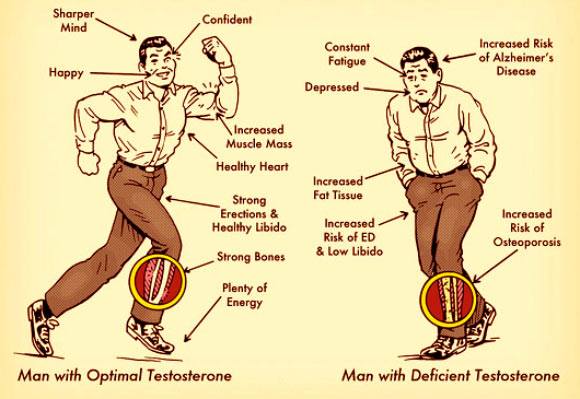
Knowledge and attitudes regarding the existence of and treatments for andropause “the male menopause” have recently undergone a revolutionary change. Andropause may consist of a variety of signs and symptoms, including:
- Loss of muscle mass and weakness
- Reduced libido
- Osteoporosis
- Heart disease and atherosclerosis
- Fatigue
- Irritability
- Insomnia
Natural Testosterone Replacement is Central to the Treatment of All facets of Andropause
The term “testosterone” is often used generically when referring to the numerous synthetic derivatives, as well as natural bioidentical testosterone. The confusion surrounding testosterone transcends the lay person; it is responsible for conflicting data in the medical literature about the benefits and risks of testosterone therapy. Studies must be reviewed carefully to determine the form of testosterone that was used. Natural testosterone must not be confused with the synthetic derivatives or “anabolic steroids”, which when used by athletes and body builders have caused disastrous effects, even resulting in heart problems and cancer. For example, administration of synthetic androgens, like stanozolol or methyltestosterone, causes profound decreases in the “good cholesterol” HDL, and significantly increases the “bad cholesterol” LDL. Yet, hormone replacement with natural bioidentical testosterone results in lower total cholesterol, lower “bad cholesterol” LDL, and with no impact on “good cholesterol” HDL.
On the average, a man’s testosterone level begins to decline at a rate of 1% per year after the age 40. Studies that measure the amount of testosterone readily available in the blood, suggest that 5% of males aged 40-50 years and 70% of the males aged 70 years have low testosterone levels. When we measure the total amount of testosterone in the blood, there is even a more marked decline with age. Some men actually go through a rather sudden change in testosterone levels that mimics the hormonal change that women experience at menopause. However, most men have a more slow and subtle hormonal decline, experiencing the same symptoms over a period of time. Blood or saliva testing is necessary to determine an individual’s testosterone level, and to establish the need for testosterone replacement therapy. Testosterone therapy is only recommended for men who have a low testosterone level. Screening for potential risks of testosterone therapy should be performed prior to the initiation of therapy. Evaluation should include history or potential history of sleep apnea, arrhythmias, obstructive benign prostatic hypertrophy, or a personal or family history of prostate cancer. When hormones are replaced back to the levels considered normal for younger males, men experience a dramatic reversal of the many changes brought about by aging.
Testosterone levels decline for a variety of reasons:
- There is less of a “signal” (Luteinizing hormone) from the brain, therefore less testosterone produced by the testes
- Testosterone producing Leydig cells in the testes begin to die off
- There is more estrogen reaching the testicles, inhibiting the production of testosterone
- The protein that binds testosterone, storing it for future use, increases with age, and binds more testosterone allowing less testosterone to be “free” and available to the cells
The diagnosis of low testosterone is made based on the signs and symptoms and the confirmed laboratory testing, which should include:
- Total testosterone (the total amount of testosterone that is in the blood, free and bound to protein)
- Free testosterone (the amount not bound to protein)
- Estradiol (estrogen)
- Lutenizing hormone (the “signal”)
Goals of Testosterone Replacement Therapy in Adult Men
- Improvement in well-being and mood
- Improvement in erectile dysfunction
- Improvement in libido
- Increased muscle mass and strength
- Preservation of bone
- Decrease in cardiovascular risk
Studies from the medical literature indicate that testosterone therapy reduces the risk of:
Osteoporosis
According to the National Osteoporosis Foundation, approximately 2 million men in the US have osteoporosis and another 3 million are at risk. Osteoporosis-related fractures occur in 12% of men older than 50. Twenty-five percent of all hip fractures occur in men, and of these men 33% will die within one year. Gradual loss of testosterone is one of the major causes of osteoporosis in elderly men. In one study, 59% of men with hip fractures had low testosterone, compared with 18% of men in the control group. Fractures occur at a later age in men than women because men’s bones are denser at baseline (from their youth). Testosterone is important to attain peak bone mass and in bone mass maintenance. Testosterone receptors are present in the cells that make bone, and testosterone is important in bone and calcium metabolism. Several studies have reported beneficial effects of testosterone therapy on bone in older men, showing an increase in bone mineral density and slowing of bone loss.
Stroke
In a study published by the American Heart Association in April 2004, ultrasounds were used to measure plaques (hardened carotid arteries) in 195 elderly men in both 1996 and again in 2000. Researchers also measured the amount of free testosterone. The results showed that men with a low testosterone level had a 3.5 times greater progression of plaque (hardening of the arteries) than those with higher testosterone. “Low free testosterone levels were related to thickening of the carotid artery in elderly men independently of other cardiovascular risk factors.
Heart disease
The risk of cardiovascular disease is decreased with men who have physiologically normal levels of testosterone, according to most reports. A number of studies have demonstrated that testosterone minimizes several important risk factors for heart disease, including:
- Reducing “bad cholesterol” LDL and reducing triglycerides
- Reducing blood sugar levels
- Decreasing fat
The degree of atherosclerotic disease (hardening of the arteries), as measured by the percent of artery occlusion, increased significantly with declining levels of testosterone. Visceral fat (fat inside the abdomen and associated with increased heart disease) is reduced by testosterone replacement. In contrast, the use of anabolic steroids including methyltestosterone (the type frequently abused by body builders) has been associated with serious heart disease.
Frailty
Frailty is defined as the condition of being frail, with generalized weakness, impaired mobility and balance, and poor endurance. Frailty is related to a decline in cognitive function as well. Low testosterone levels have been found to predict frailty in males.
Alzheimer’s disease
Testosterone replacement therapy improves verbal memory, working memory, and visuospatial performance in men. (Neurology 2001 Jul 10;57(1):80-88).
Two interventional studies have supported the concept that testosterone can improve cognitive function in older men. Testosterone plays an integral role in the age-related cognitive impairment that occurs in males and low testosterone levels play a role in the pathogenesis of Alzheimer’s disease.
Gandy, et al, in a landmark study showed that the levels of circulating amyloid-peptide (the main toxin to brain cells in Alzheimer’s disease) is under the control of gonadal hormones, and suggests that testosterone replacement therapy might prevent or delay Alzheimer’s disease in men.
Depression
Measurements of depression are higher when testosterone is low; perhaps because of an associated decrease in sexual function results in depression, irritability, and mood swings. IN the Rancho Bernardo Study which examined the association between levels of sex hormones and depression, testosterone levels were 17% lower for depressed men. The results suggest that testosterone therapy might improve depression in older men who have low levels of testosterone.
Symptoms of testosterone deficiency are often attributed to other problems, denied by the patient, and unrecognized by the physician. Testosterone is necessary for erections, normal libido, and ejaculation. The Massachusetts Male Aging Study reported that low testosterone is the sole cause of erectile dysfunction (impotence) in 10% of cases. Unfortunately, many of these men and their physicians will not be aware of the cause and the option of treatment using natural testosterone. Instead, they resort to other forms of therapy with the potential for side effects, such as the use of Viagra, rather than experience the many benefits of natural hormone replacement therapy.
Testosterone and Prostate Cancer
Of the 27 medical studies published on the relationship between testosterone and prostate cancer, only five studies indicate that men with higher testosterone levels had a greater risk of prostate cancer, whereas 21 of the studies show testosterone was not a risk factor, and one study is considered neutral. In a study published in January 2004, 708 testosterone levels in men with prostate cancer were compared to 2,242 men without prostate cancer. The results showed that higher levels of testosterone correlated with a decreased risk of prostate cancer. In fact, men with the highest free testosterone levels were 18% less likely to have prostate cancer than men with the lowest levels.
What is the best form of Testosterone for Replacement Therapy?
A healthy male secretes 8-15mg/day of testosterone. Low testosterone levels are associated with all the symptoms listed above of andropause “the male menopause”, but high testosterone levels which can occur when replacing testosterone results in some serious side effects such as an increase in estrogen levels (testosterone is converted to estrogen when testosterone is present in high amounts) and an increase in Dihydrotestosterone (DHT). High estrogen levels can lead to a diminished libido or breast swelling. High levels of DHT have association with benign prostatic hypertrophy.
There are various forms and methods of increasing testosterone levels. Some of the more common and safer methods are listed:
Testosterone cream
Testosterone cream is natural bioidentical testosterone that has been approved by the United States Pharmacopoeia. The advantage of testosterone cream is that it can be applied daily to insure daily maintenance of testosterone without the associated peaks and valleys of weekly injections. There has been some concern that transdermal (cream) testosterone may increase estrogen levels, but the newer creams developed by compounding pharmacies have shown to be safe and effective in increasing testosterone without the associated increase in estrogen. The problem with cream is that it needs to be applied daily, can be transmitted to other people through touch if not allowed to dry properly, and may not be able to be given in sufficient amount to increase the testosterone level to the desired effect.
HCG “the signal”
Human Choriogonadotropin is an injectible form of the hormone that stimulates the testes to produce testosterone. In this manner, you can safely raise your own production of testosterone. This does require the injection of medication, similar to the manner in which diabetics give themselves insulin.
Testosterone Cypionate
This injectible form of natural testosterone safely and effectively raises the testosterone level once the testes cannot longer be stimulated to produce testosterone. This form is released over the course of a few days, and maintains a level in the blood for up to 10 days. Injected usually once a week, this form of replacement therapy is reserved for last resort; it requires an intramuscular injection that most men would rather not undergo.
Testosterone pellets
The natural form of testosterone requires the physician to implant a pellet of testosterone in the buttock area, for slow release over the course of 3 months. This form can have lower effects on estrogen conversion, but it does not allow for modification of the dose. Once implanted, it remains for 3 months without the ability to alter or modify the dose.
The only absolute contraindication to testosterone replacement is the presence of prostate or breast cancer. “Although it is know that he clinical course of prostate cancer is accelerated by testosterone, its incidence is NOT increased by testosterone administration… there is even no clear evidence that testosterone replacement accelerates the development of benign prostatic hypertrophy” Drug and Aging 1999 Aug;15(2):131-42
HEALTHY LIFESTYLE
Testosterone levels decline at a steady rate of about 1-2% per year after the age of 25. The Massachusetts Male Aging Study revealed that testosterone levels in 1,709 men aged 39-70 years showed that good health among aging men correlates with higher levels of testosterone.
When hormone levels decline, we become less active and gain weight. As we gain weight, hormones are stored in fat and become unavailable to meet the body’s demand. Lack of exercise, excessive alcohol use, and many diseases can reduce hormone levels. For optimal results, it is vital that hormone replacement therapy be combined with adequate exercise, proper nutrition, and appropriate use of natural supplements.